Once the alcohol gets to the stomach, most of it is sent to the liver for processing. In very small amounts alcohol is less harmless. But if a person uses alcohol in excess then it can lead to serious liver complications. So, this is the main cause of liver disease in western countries.
What are the symptoms of Alcohol-related liver disease?
- Lack of nutrients
- Excess waste products presented in your blood
- Fatigue
- Loss of appetite
- Yellowing of the skin
- Swelling of the abdomen
- Internal bleeding
- Confusion
- Kidney failure
are common these symptoms may vary depending on the stage of your alcohol-related liver disease.
What are the 3 stages of Alcohol-related liver disease?
Alcohol-related liver disease has three stages. Keep in mind that there can be an overlap of stages. If it diagnosis early so it can reverse the liver damage.
Stage 1: Fatty liver or Steatosis:
The most common and earliest stage of alcohol-related liver disease is called fatty liver or steatosis. Fatty liver refers to an excess buildup of fat inside of the liver cells. This makes it harder for the liver to function.
Symptoms in this stage are often few but experiencing general fatigue and weakness are common. This buildup of fat inside the liver cells can also result in an enlarged liver called hepatomegaly. This condition causes discomfort or pain in the upper right side of the belly. So high usage of alcohol can cause fatty liver. Typically the fat inside of the liver will lessen once a person stops drinking
Stage2: alcoholic hepatitis and alcoholic steatohepatitis:
Stage two of alcohol-related liver disease refers to swelling or inflammation of the liver. So, liver cell damage is known as alcoholic steatohepatitis or alcoholic hepatitis.
- Abdominal pain
- Fever weakness
- Nausea
- Vomiting
- Loss of appetite
- The yellowing of the eyes and skin
are common symptoms alcoholic hepatitis. It can be mild or severe. In its severe form the disease occur suddenly and cause life-threatening complications.
Stage 3: severe alcoholic hepatitis and alcohol-related cirrhosis:
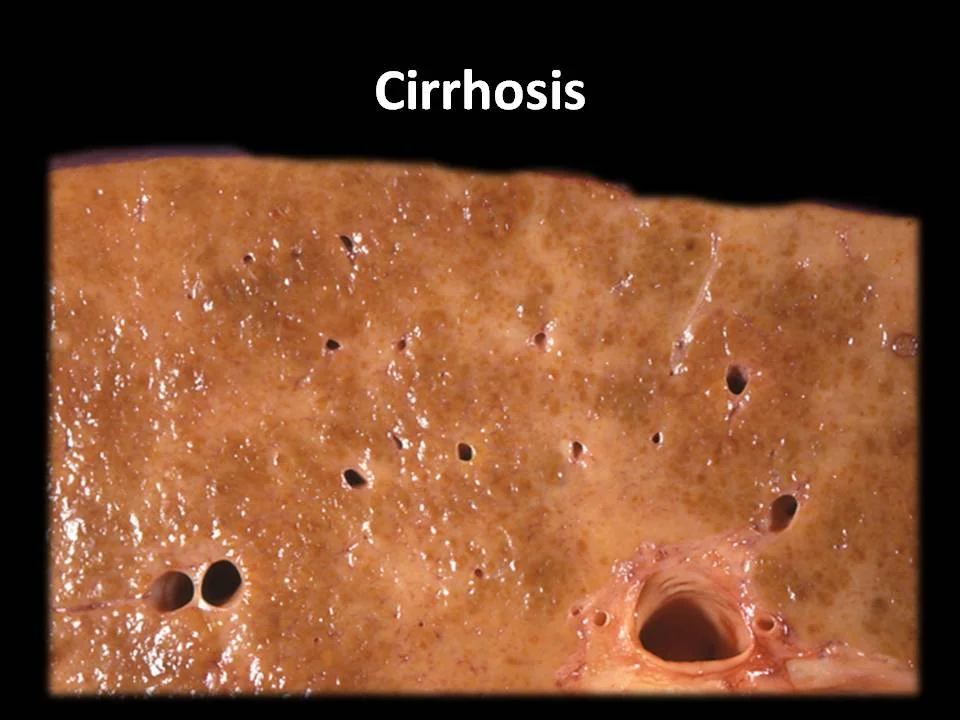
Severe alcohol-related cirrhosis and alcoholic hepatitis are the most serious stages of alcohol-related liver disease. Anything that damages the liver over many years can cause the development of scar tissue in the liver. Liver scarring first stage is name fibrosis. When scar tissue builds up significantly and takes over most of the liver it is referrs to as cirrhosis.
Symptoms of cirrhosis include:
- High pressure in the portal vein
- An enlarged spleen
- Fluid buildup in the belly
- Internal bleeding
- Confusion

How to diagnosis alcoholic liver disease?
Early diagnosis of alcohol-related liver disease can be challenging. Because its symptoms and signs are mild in the early stages. If the doctor suspects potential damage to the liver due to alcohol they will typically arrange blood tests and an ultrasound to check on how well the liver is working. A doctor will check a person’s alcohol consumption. Some tests such as a CT scan, an MRI, or a liver biopsy also suggest. All these tests may be helpful in examining the liver for potential injury or damage.
What happens to your liver if you drink alcohol every day?
Pathways of alcohol in the liver:
When alcohol goes into the liver cells or hepatocytes so it can take three pathways:
- One of which involves an enzyme called alcohol dehydrogenase or simply ADH, and this happens in the cytosol of the cell
- Another involves a catalase inside organelles called peroxisomes
- The third pathway involves an enzyme name cytochrome P450 2E1
In all three pathways, alcohol is converting into acetaldehyde.
Why liver color is more yellow?
When the ADH enzyme is utilize for the conversion of the alcohol so it also needs another compound called NAD+. So, NAD+ is then converts into NADH. As a result NADH levels increase. And at the same time, NAD+ levels decrease. So, this has two effects, first it higher the level of NADH and also tells the cell to start producing more fatty acids. And second, it lowers the NAD+ levels which results in less fatty acid oxidation.
As a result, both of these lead to more fat production in the liver. An excessive amount of fat in the liver is also causes fatty liver. So due to this liver gets large, tender, greasy, and heavy. At this point, patients don’t have symptoms like high levels of neutrophils in the blood and fever. The liver color is more yellowish due to all the fat deposits. This increase amount of fat in the liver is referrs to as steatosis.
What are the functions of acetaldehyde formed after alcohol metabolism?
When acetaldehyde is formed from ethanol, it will generate compounds called reactive oxygen species. For example hydrogen peroxide, the hydroxyl radical, or the superoxide anion reacts with different components of the hepatocyte, DNA, and proteins. So, this process causes serious damage to the cells.
Secondly, acetaldehyde also binds to macromolecules, enzymes, the cell membrane, and all sorts of other compounds inside the cell. When they bind to some of these, they effectively inhibit that molecule. And when that happens, they form the compound called acetaldehyde adducts.
And when those are formed, the immune system recognizes these new compounds as foreign and starts sending neutrophils in to sort of clean up the damage. So, the destruction of hepatocytes by neutrophilic infiltration occurs.
As cells become inflamed and damaged, patients have developed alcoholic hepatitis, and a person starts to note a change in histology and notice these bundles of proteins called Mallory bodies. The mechanism that produces these bodies is still unclear, but they’re most commonly sees in alcoholic hepatitis.
At this point the patient may have hepatomegaly that’s probably become painful since the liver’s seeing more immune cells, they also may have neutrophilic leukocytosis or increased neutrophils in the blood. Also, as cells become damaged and die off, scar tissue starts to form around the central veins in the liver, known as perivenular fibrosis.
The damage done to hepatocytes also results in leakage of liver enzymes like alanine aminotransferase (or ALT) or aspartate aminotransferase (or AST), both types of transaminase,
Usually, even though both are elevated, AST will be greater than ALT in alcoholic hepatitis. In addition to these two, serum alkaline phosphatase (or ALP) and gamma-glutamyltransferase (or GGT) will also be elevated.
In some cases, thrombocytopenia, a deficiency of platelets in the blood as well as possible hypoglycemia, or low blood sugar, can also be found in the blood of someone with alcoholic liver disease.
What is the treatment for alcoholic liver disease?
Treatment again involves completely stopping alcohol consumption, and in some cases, corticosteroids can help suppress the immune system.
Summary:
People with cirrhosis have an increased risk of developing liver cancer as well as the need for a liver transplant. People with already liver disease have a great chance to develop liver damage and cirrhosis. It is strongly recommends that if a person is living with any form of liver disease not drinks alcohol.